The rushing vortex of siren and light is a familiar cue: Get out of the way, halt. Then we move on without giving much thought to the patient in transit, nor to the possibility that a casual trip of our own could turn into a hospital emergency.
“I think when you get in your car in the morning to go to work or on your way home or whatever, you would never think … that, even more than your marriage, it becomes this distinguishing moment in your life,” said Wesley Wride, who worked as a trauma technician in the Emergency Department at the University of Chicago from 2021 to 2023. With 911 dispatching ambulances to 1.5 million traffic crashes annually in the United States, emergency medical service and emergency room professionals know better than most the raw significance of automobile violence.
Car crashes occupy space where acute public health concerns and road safety planning overlap. Response time and quality treatment make up “Post-Crash Care,” a pillar of the “Safe System Approach,” to which the US Department of Transportation officially subscribes.
When the first four pillars — Safer People, Safer Vehicles, Safer Speeds, and Safer Roads — fail, and they often do, the enormous real-time responsibility of keeping people safe and alive falls on trauma care professionals.
As one paramedic with ample experience on private ambulances in the St. Louis area told me, that responsibility comes with great risk.
Firstly, she told me, the use of emergency lights and sirens to run red lights on hostile thoroughfares presents a series of perilous decisions. Then, once the patient is strapped in, she explained, paramedics often forgo buckling up themselves.
“You can't always reach your monitor. You know, you're running wires and medications all over the place,” said the paramedic, who spoke on the condition of anonymity. “ If you're doing CPR and intubation, that obviously requires movement. So there's an inherent risk to the paramedics by being unbuckled in the back of an ambulance in the event of a potential accident.”
In fact, ambulance workers are 3.6-times more likely to suffer transportation-related injuries. In 2020, the overall injury rate for paramedicine professionals was more than four-times the national average for all US workers. The rate was higher for women than for men.
In one instance, the paramedic told me, she and a colleague responded to a flipped car on the side of a country road, slick with rain from the night before. The road had no shoulder, and they had to park within the lane. While the car’s occupant walked away unscathed, and they pulled away without a patient, another driver hurtled around the curve, hitting the ambulance head-on and totaling it. The paramedics were okay, but the people in the opposing car had to go to the emergency department.
My source recalled another story of an acquaintance she felt clarified the stakes of her work.
Erik Bedwell was tending to an overdose patient in an ambulance traversing Interstate 55 near Pevely, Missouri when a drunk driver in a Jeep Grand Cherokee swerved from the oncoming lane and struck the vehicle. The ambulance careened off road and flipped, leaving Bedwell with a severed spinal cord. He’s now paralyzed from the waist down. The driver and patient suffered less severe injuries.
Paramedics also endure secondary traumas.
“I've seen some really bad accidents and things that have been more traumatic for me,” my source told me, “...with either people not wearing their seatbelts in cars or people in motorcycles not wearing helmets … I wish that people would not take those things so lightly.”
Car crashes make up more than a quarter of all causes of injuries that EMS respond to. A huge amount of resources are deployed when paramedics transfer care to emergency departments. Each trauma patient receives a full body assessment. Their bodies must be logrolled to prevent movement of the spine, a CT scan is taken to assess injuries to spine and head and a full neurological evaluation is completed.
When a crash victimizes multiple people, the influx may require emergency departments to pull staff from other patients. Crashes “take attention and time and energy from other patients who are coming in with other issues,” Wride, the former Chicago trauma technician told me.
Wride also described particular difficulties of treating crash victims. Wounds from motor vehicle crashes, he said, tended to be larger, more widespread and more horrific than wounds from falls, physical assault or even gun violence. Then there is the volume of people who don’t survive: Of the 42,939 people who died in car crashes in the US in 2021, 40 percent died after EMS arrived.
Creating emotional boundaries, unsurprisingly, is necessary for trauma care professionals to make clear, rational decisions that best serve patients in dire circumstances. Coping in the aftermath is another matter.
“All these things that are very heavy, things that we’re, you know, right up close with, we get very used to kind of pushing aside and not recognizing, because we have three or four other patients … we don't exactly always have time to sit and linger in those feelings,” Wride said.
It wasn’t until after Wride left his position in the emergency department to attend medical school that he said he felt a burden was lifted.
Alex Pennington, a nurse at a level one trauma center in St. Louis County, described one challenge in constructing those emotional boundaries.
“As a cyclist myself I kind of have a special place for any cyclist that gets hit. That’s one of my soft spots,” he told me.
Pennington bikes 15 miles to work once a week. It's a tool to help him cope with work-related stress.
His experiences have led him into documenting bike and motorcycle crashes by photographing victims’ helmets (if and when they can consent), as well as advocating for more protected bike lanes, infrastructure that might keep more travelers from getting injured by cars—and out of the hospital.
“[Cycling is] just a huge part of my mental health strategy,” he said “It’s become a big part of my social life, and that’s something I want to share with my daughter safely. Sometimes just, in St. Louis, it doesn’t feel like we’re there quite yet, and it still really scares me.”
Reactive and Proactive Care
I asked Pennington what he wished the public knew about his work. He was quick to mention high rates of turnover for emergency professionals and the high level of violence they face.
In one survey, 70 percent of emergency room nurses reported that they had faced physical assault. In a society where primary care can be elusive, shelter for unhoused individuals scarce and public psychological turmoil has risen in recent years, the emergency department, open to all, tends to absorb all the societal ills we aren’t addressing proactively. Automobile violence, with its endless intersections, is just one on a long list.
A recent review of pre-hospital care for crash victims found that despite a “Decade of Action for Road Safety” in the public policy space, limited changes to pre-hospital care made little-to-no difference on patient outcomes or fatalities between 2011 and 2020. The researchers pointed to the “ever-increasing number of people relying on motor-vehicle transport” and “the inability of governments and organizations to consider a systems approach to road-traffic safety as opposed to examining individual interventions.”
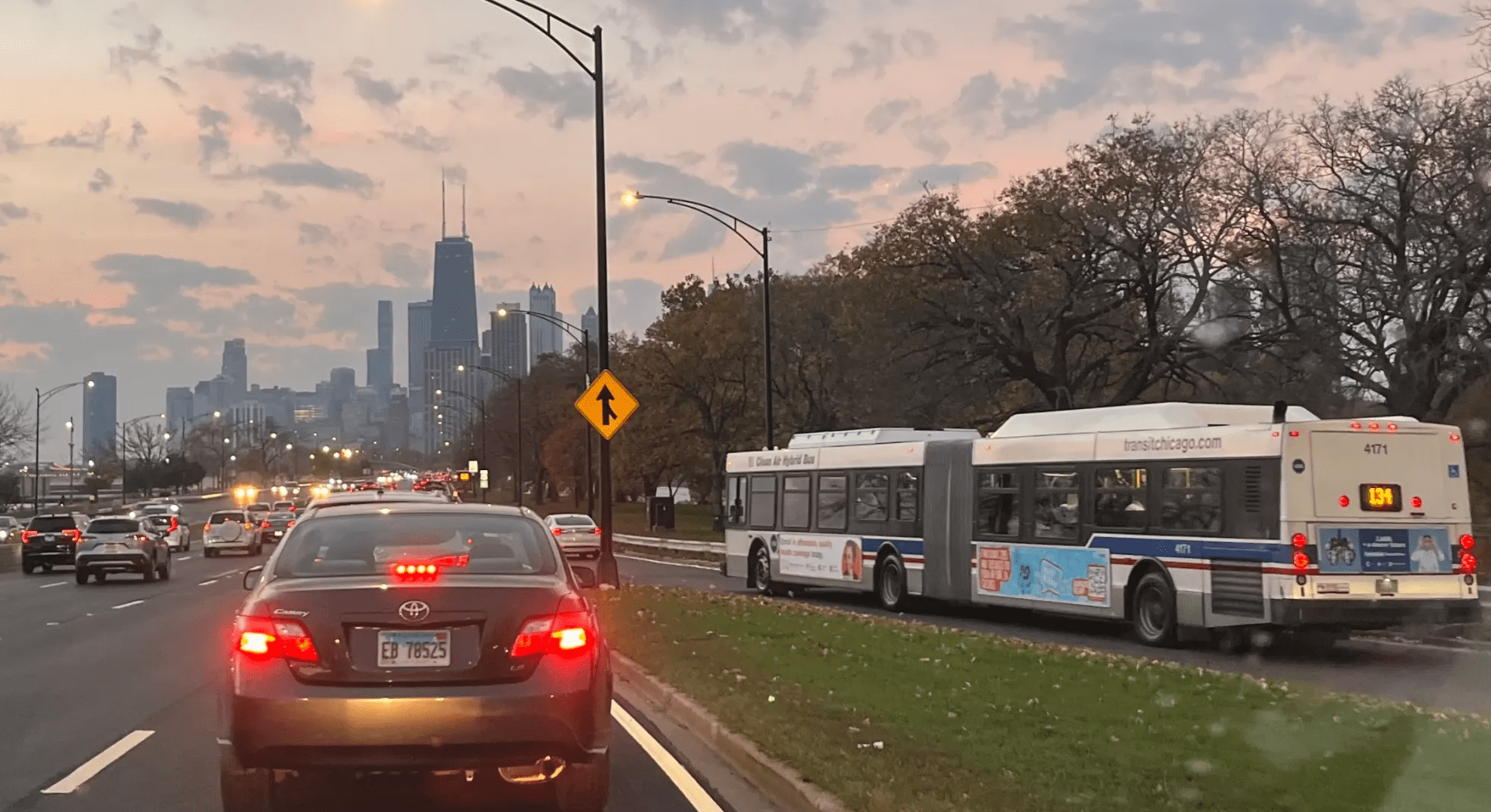
In other words, safety does not increase if we ask emergency medical professionals to arrive faster to crash sites or provide higher quality care, but driving keeps growing. Increasing options for people to walk, bike and take public transit on roads where drivers must drive more slowly and patiently just might keep us out of ambulances and emergency departments. In turn, less crashes might offer relief to those who choose to treat our abundant ills. Mobility and public health are enmeshed, and, as the old proverb goes, an ounce of prevention is worth a pound of cure.